Sad tale of the Toronto Academy of Medicine
The Toronto Academy of Medicine exists as a "shell" in a storage room at SUNNYBROOK Hospital in North Toronto. There is money deposited from the sale of the 288 Bloor building, the interest is used for a free yearly dinner lecture meeting at the VAUGHAN ESTATE donated to Sunnybrook Hospital. The acting President is Ophthalmologist John FOWLER MD(Tor.1958) FRCSC(1972) of 199 Golfdale road, Toronto M4N 2B7.Te:416- 483-5106.. The Academy has lost its Charitable status. There is no yearly AGM. .Recently Dr.Fowler commissioned Academy ties in Blue & Red. With support from the profession & industry, the Academy could be restored to its former important role in Toronto Medicine.
06 January, 2011
The Scientist ( HARVARD Drs Aaron BERNSTEIN & Samuel S. MYERS)
DIRECT IMPACTS OF CLIMATE CHANGE Infectious Disease • Climate change will alter the distribution of malaria, dengue fever, schistosomiasis, and others that are transmitted by an insect vector or those that have animal reservoir hosts. • The range of these diseases is limited geographically by the range of the insects and/or animal reservoirs that effect their transmission to humans. As temperature and precipitation patterns change, so too will the geography conducive to the survival of these other species. • Warming temperatures increase the rates of reproduction, development, survival, and biting of blood-feeding vectors as well as shortening the parasite development time inside these vectors. • Geographic shift from one locale to another may introduce pathogens into novel and nonimmune human populations who may be far more susceptible to infection than those now living in endemic areas. Heat Stress • Increased extreme heat events can exact a heavy human health toll. • Hyperthermia may cause relatively mild illness such as heat rash, exhaustion, or heat syncope (fainting), but may also precipitate severe sequelae including heat stroke, which is often fatal. • Survivors of heat stroke experience a marked increase in illness and mortality in years subsequent to the extreme heat event. • An additional 2.5 billion people will be added to the planet’s population over the next 40 years and nearly all of them will live in cities. Cities tend to be warmer due to the urban heat-island effect. • The human population is aging, and the elderly are particularly sensitive to heat stress. Air pollution • The formation of ground-level ozone, the major cardiorespiratory toxin in smog, is coupled to temperature particularly as temperatures rise above 90°F (32°C). • Climate change has brought about an earlier start to spring and later end to fall, and these changes to seasonality, along with higher CO2 concentrations, yield both longer pollen seasons and more pollen production from many allergenic plants. • Allergic respiratory disease, particularly asthma, is already associated with a quarter of a million deaths annually worldwide. • The frequency and extent of forest fires is expected to rise, generating large amounts of air pollutants, including potent lung irritants (such as acrolein and other aldehydes), carcinogens (such as formaldehyde and benzene) and fine particulates (PM 2.5) which are known to increase risk of cardiorespiratory disease and death. Living with uncertainty There is no doubt that climate change will have important impacts on human health, but we are uncertain about what those impacts will be and where and when they will be most severe. The most consequential health effects of climate change will come about from interactions between biophysical changes to the natural environment, demographic trends, and human adaptations. (See Figure 3) The biophysical changes—such as temperature variability or sea level rise—are difficult to predict with accuracy today, and the capacity for adapting to these changes is largely unknown. 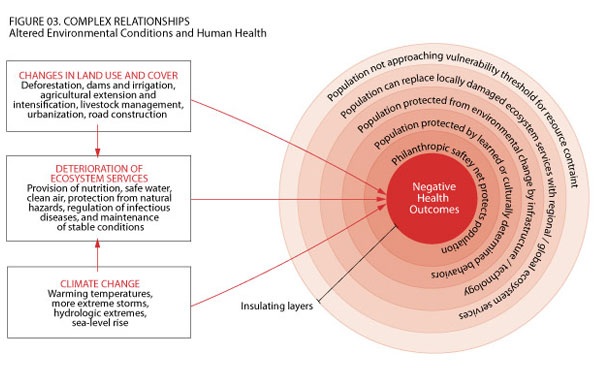 Click for larger image But uncertainty about the exact timing, location, or magnitude of climate change impacts is no excuse for complacency. With evidence that climate change is already imposing a hefty health burden, the future climate, particularly if greenhouse-gas releases into the atmosphere go unabated, portends health crises for hundreds of millions of people. Rather than be used as a rationale for inaction, the uncertainty inherent in climate science should serve as an organizing principle for adaptation to its ill effects. For example, uncertainty about future viable regions and conditions for agriculture requires a variety of new crop strains with traits such as heat and drought resistance. Changes in the timing of seasonal flow from melting snow pack or glaciers call for a dramatic increase in water-storage capacity for people depending on these flows for household use or irrigation. Insurance schemes allowing different countries or populations to pool their risk of crop failure and food insecurity might be enacted to blunt the toll of regional climatic disruption. Surveillance efforts should be designed that allow us to better detect changing distributions of infectious disease, water scarcity, or food insecurity early on so that resources can be efficiently redirected............ Faculty Member Samuel S. Myers is an instructor in medicine, Harvard Medical School; research associate, Harvard University Center for the Environment; and staff physician, Mount Auburn Hospital. Aaron Bernstein is a faculty member at the Center for Health and the Global Environment; instructor in pediatrics, Harvard Medical School; and physician in medicine at Children’s Hospital Boston. 1. Intergovernmental Panel on Climate Change (IPCC), “Climate Change 2007: Impacts, adaptation and vulnerability. Contribution of Working Group 2,” Intergovernmental Panel on Climate Change (IPCC), 2007. 2. F.C. Curriero et al., “The association between extreme precipitation and waterborne disease outbreaks in the United States, 1948-1994,” Am J Public Health, 91:1194-99, 2001. 3. D.S. Battisti, R.L. Naylor, “Historical warnings of future food insecurity with unprecedented seasonal heat,”Science, 323:240-44, 2009. Free F1000 Evaluation 4. D.B. Lobell et al., “Prioritizing climate change adaptation needs for food security in 2030,” Science, 319:607-10, 2008. 5. S. Peng et al., “Rice yields decline with higher night temperature from global warming,” PNAS, 101:9971-75, 2004. 6. L.E. Caulfield, R.E. Black, “Zinc Deficiency,” in Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors, Vol. 1, M. Ezzati, et al., eds, Geneva: World Health Organization, 2004, pp. 257-79. 7. R.J. Stoltzfus, L. Mullany, R.E. Black, “Iron Deficiency Anemia,” in Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors, Vol. 1, M. Ezzati, et al., eds, Geneva: World Health Organization, 2004, pp. 163-209. 8. L.C. Johnstone, “Planning for the inevitable, the humanitarian consequences of climate change,” in “Linking Climate Change Negotiations and Disaster Risk Reduction” Copenhagen, 2008. 9. K. Warner et al., “In search of shelter: mapping the effects of climate change on human migration and displacement,” Cooperative for Assistance and Relief Everywhere (CARE), New York, NY, 2009. 10. M.J. Toole, R.J. Waldman, “Refugees and displaced persons. War, hunger, and public health,” JAMA, 270:600-05, 1993. 11. L.A. McCloskey, K. Southwick, “Psychosocial problems in refugee children exposed to war,” Pediatrics, 97:394-97, 1996. Advertisement Rate this article
|
 Register for FREE Online Access
Register for FREE Online Access
- »Current issue
- »Best Places to Work and Salary surveys
- »Daily news and monthly contents emails
 Subscribe to the Magazine
Subscribe to the Magazine
- »Monthly print issues
- »Unlimited online access
- »Special offers on books, apparel, and more
Read more: The Coming Health Crisis - The Scientist - Magazine of the Life Sciences http://www.the-scientist.com/article/display/57882/#ixzz1AJXw825D
Subscribe to:
Post Comments (Atom)


No comments:
Post a Comment